Abstract
BACKGROUND AND AIMS
Diffuse Large B Cell Lymphoma (DLBCL) is an heterogeneous group of diseases whose behavior can be predicted by clinical risk scores, immuno-histochemistry and cytogenetic. Among DLBCL, patient with high risk features such as high IPI score, high mitotic index, double hit lymphomas display a worse outcome and the standard frontline treatment with R-CHOP usually results in poor outcome. Consequently, many groups have explored more intensified first line regimens for those patients, such as R-DA-EPOCH and R-CODOX-M/IVAC-R.
However, no study directly comparing conventional R-CHOP with more aggressive regimens are currently available, so that a clear indication of superior efficacy from an intensified approach has not been provided yet.
The aim of the present was to retrospectively compare through a match-paired analysis two cohorts of patients affected by aggressive DLBCL who were treated with either conventional R-CHOP (center 1) or intensified R-CODOX-M/IVAC-R (center 2) as frontline regimen, in order to disclose to identify subgroups of patients who are more likely to benefit from intensive first line approach.
PATIENTS AND METHODS
High Risk DLBCL was defined by at least one among these features: high tumour burden, DPLs, IPI score >3 or the presence of at least 1 extranodal site.
In center 1, 6 x R-CHOP is standard therapy for every patient with newly diagnosed DLBCL, whereas in center 2 patients with aggressive DLBCL are treated with R-CODOX/IVAC-R repeated for two courses.
Fifty-one patients affected by aggressive DLBCL and treated with R-CHOP or R-CODOX-M/IVAC-R between January 2011 and January 2015 in the two centers were retrospectively included in a match-paired analysis. Median follow up was 36 months.
Matching variables were age, IPI score, disease staging according to Ann Arbor, cell of origin according to Hans algorithm. Matching ratio was 2:1 (2 patients treated with conventional R-CHOP were matched with each patient treated with R-CODOX-M/IVAC-R).
The two groups of patients had no significant differences in baseline characteristics such as age, stage, IPI and cell of origin.
To disclose differences in terms of efficacy, overall response rate, as defined by international standard, overall survival and cumulative incidence of relapse were compared between the two cohorts.
RESULTS
Overall response rate (ORR) was 44/51 (86.3%). Patient treated with R-CODOX-M/IVAC-R had an higher probability to achieve at least a partial response (17/17, 100%, vs 27/34, 79.4%, p<0.05, respectively for R-CODOX-M/IVAC-R and R-CHOP).
Specifically, after a subgroup analysis, patients with age <50 yrs (p<0.05) and stage III/IV (p<0.05) were found to have a significant improvement in ORR if treated with R-CODOX-M/IVAC-R. A trend towards improved chance of response with R-CODOX-M/IVAC-R, however without reaching statistical significance was observed among patients with germinal center DLBCL, according to Hans algorithm.
Overall survival (OS) at 3 years was 88.2% (median of reached) and was not significantly different among patients treated with R-CHOP (3 year OS=86.9%) or R-CODOX-M/IVAC-R (3-year OS=93.2%). None of the other analyzed variables significantly impacted OS probability.
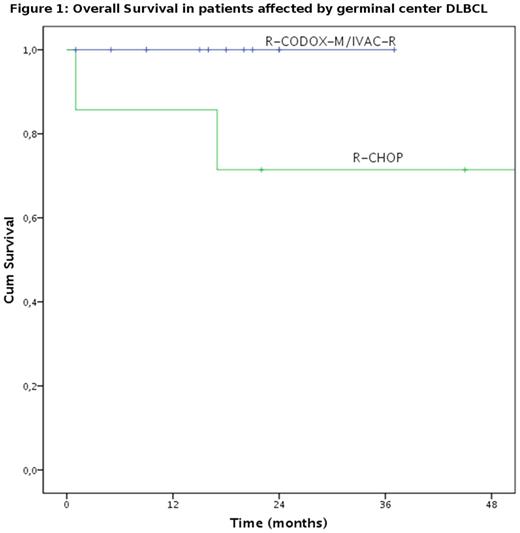
After subgroup analysis, a trend for improved OS if treated with R-CODOX-M/IVAC-R was found among patients with IPI score >3, age <50 and germinal center DLBLC (Figure 1), again without reaching statistical significance.
Patient treated with R-CODOX-M/IVAC-R had a significantly higher probability of experiencing grade III/IV hematological toxicities (p<0.05), grade III/IV mucositis (p<0.05) or grade III/IV infections (p<0.05), whereas cardiovascular and hepatic toxicities were unlikely and non significantly different among the two cohorts.
CONCLUSIONS
R-CODOX-M/IVAC is an highly effective regimen for patients affected by DLBCL, with an ORR significantly higher than conventional R-CHOP, however at the price of significantly higher therapy-related toxicities. Our results seem to suggest a potential benefit for younger patients with very aggressive DLBCL, where higher risk of toxicities is overcome by the improved probability of cure.
Of note, patient with germinal center DLBCL seem to take a greater benefit from the intensified approach, this may be explained by the higher chemo-sensitivity that is usually observed in this setting, however our result must be confirmed in larger trials.
Bocchia: Jansen: Other: Travel grant; Novartis: Other: Travel grant; Celgene: Other: Travel grant; Roche: Other: Travel grant.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal